Pressure Ulcer Care: Causes: diagnosis and treatment
Imagine lying immobile for hours, unaware that your skin is slowly succumbing to a preventable injury known as a pressure ulcer. These painful wounds, often seen in individuals with limited mobility, can lead to serious complications if not addressed promptly. Understanding pressure ulcers, their causes, symptoms, and treatment is essential for both patients and caregivers alike.
Pressure ulcers, also referred to as bedsores, occur when prolonged pressure on the skin reduces blood flow, damaging the tissue. Factors contributing to their development can be intrinsic, such as age and health conditions, or extrinsic, including moisture and friction. Awareness of the various stages of these ulcers, from early signs to advanced symptoms, is crucial for timely intervention.
Definition Pressure Ulcers
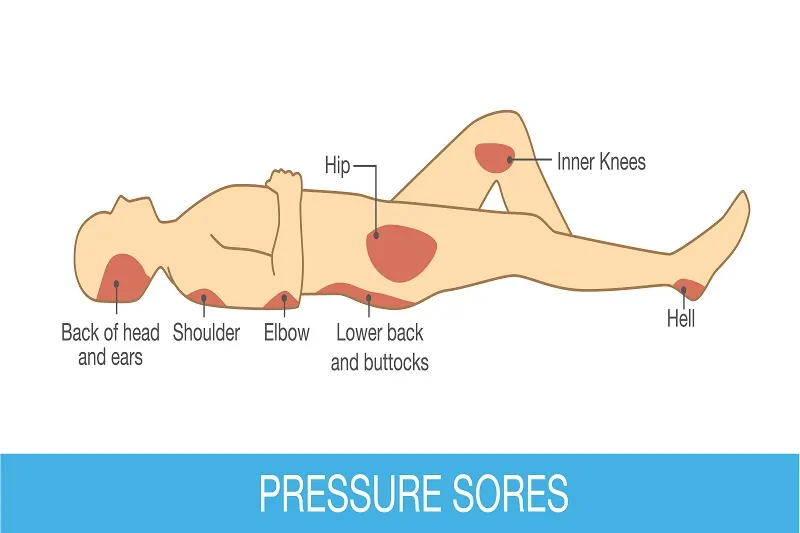
Pressure ulcers, or bedsores, are injuries to the skin and tissue beneath it. They occur when there's prolonged pressure on the skin. This often happens on bony body parts like heels, elbows, hips, and the tailbone. These ulcers form due to reduced blood flow, which can lead to tissue damage or even tissue death.
People with limited mobility are at higher risk for pressure ulcers. This includes the elderly, those with serious illnesses, and patients in intensive care. Conditions affecting sensation, circulation, or skin integrity also increase the risk. When a person cannot move easily, their body weight puts constant pressure on certain skin areas.
Every year, over 2.5 million people in the U.S. develop pressure ulcers. This not only causes pain but can also lead to serious infections. Because of this, treatment often requires more healthcare resources.
To treat pressure ulcers, a range of methods is used. Care might include special mattresses, cushions, and dressings. In severe cases, surgery may be needed to clean and close the ulcer.

Preventing pressure ulcers is very important. It involves changing positions regularly and checking the skin every day. A healthy diet also helps, along with using supportive devices to take away pressure from vulnerable areas.
Signs and Symptoms of Pressure Ulcers
- Discolored patches of skin that do not change color when pressed
- Warmth or hardness in the affected area
- Blisters or open wounds in advanced stages
By knowing these signs, early detection and treatment are possible, reducing the risk of complications. Prevention and management must be part of daily routines for those at risk.
Understanding Pressure Ulcers
Pressure ulcers, also known as bedsores or pressure sores, are skin injuries caused by prolonged pressure on the skin. This pressure can reduce blood flow, leading to dead tissue and other complications. Individuals with limited mobility, such as the elderly or those with a spinal cord injury, are at a higher risk of developing pressure injuries.
These injuries often occur in areas where the bone is close to the skin, like the elbows, heels, and hips. High-risk groups include patients in intensive care and people with conditions that affect sensation or circulation.
To prevent these ulcers, it's important to change positions regularly and perform daily skin assessments. A healthy diet and proper nutrition, focusing on a positive nitrogen balance, can also help maintain intact skin. Supportive devices, like specialized mattresses and foam dressings, can relieve pressure and aid in the management of pressure ulcers.
Treatment can range from simple care to surgical interventions like skin grafts. Early detection of signs of infection and maintaining a moist wound environment are crucial for healing. Managing chronic and deep wounds may require more advanced therapies, such as Hyperbaric oxygen therapy or antibiotic treatment, especially if bacterial infections occur.
Causes and Risk Factors of Pressure Ulcers
Pressure ulcers develop due to several causes and risk factors. Prolonged pressure on the skin is the primary cause, as it restricts blood flow and leads to tissue damage. Individuals who can't move well, like older adults, face a higher risk since they cannot change positions as needed. Conditions like urinary or fecal incontinence expose skin to irritants, increasing ulcer risk. Malnutrition weakens the skin and blood supply, elevating the chance of breakdown. Poor circulation and sensory issues, such as nerve damage, hinder the response to discomfort, making pressure sores more likely.
Intrinsic Factors
Intrinsic factors are those related to the body itself. Advanced age is a significant factor, as older adults have thinner skin that heals more slowly. Impaired sensation from conditions like diabetes prevents noticing discomfort, enhancing ulcer risk. Malnutrition causes the skin to thin and the blood supply to weaken, slowing healing. People with medical conditions like paralysis often decrease mobility, leading to ulcers. Additionally, conditions like peripheral arterial disease reduce blood flow to the skin, increasing injury risks.
Extrinsic Factors
Extrinsic factors are external influences that contribute to pressure ulcers. Prolonged pressure from surfaces, such as beds or wheelchairs, can damage the skin. Long-term exposure to irritants like urine or feces also raises the risk. Aging skin is delicate, making older adults more prone to sores during immobility. Reduced blood flow, due to circulation issues or obesity, can increase ulcer risks. Smoking affects skin blood flow, further raising the possibility, especially in those with limited movement.
Here's a list of some extrinsic factors to consider:
- Prolonged pressure from surfaces
- Exposure to skin irritants (urine/feces)
- Delicate skin in older adults
- Poor circulation and obesity
- Smoking and its impact on blood flow
Symptoms of Pressure Ulcers
Pressure ulcers, also known as bedsores or decubitus ulcers, are injuries to the skin and underlying tissues from prolonged pressure. Recognizing the symptoms early
Early Signs of Pressure Ulcers
The first signs of a pressure ulcer often include skin redness that does not fade when you press it. This can be an early warning that the skin is starting to suffer damage. A patch of skin that feels warm, spongy, or harder than the surrounding skin can also be an early sign.
Itchiness or pain in the area might indicate skin damage is beginning. Look for discolored skin that does not change with pressure. On lighter skin, this may appear red; on darker skin, it could look blue or purple. Regular checks for these signs are vital, especially around bony areas such as heels, hips, and the tailbone.
Advanced Symptoms
As pressure ulcers progress, they can form deep, crater-like sores. These may show signs of infection, such as red edges, pus, unpleasant odors, and drainage. Sometimes, the tissue around these sores may appear black, signaling dead tissue, known as necrosis. Stage IV pressure ulcers are very serious. They can damage not only skin but reach deep enough to harm muscles, ligaments, and even bones.
Tendons or muscles might be visible in extreme cases. In some cases, the depth of the sore is hidden by a layer of dead tissue, making it unstageable without medical treatment. A deep tissue injury can also appear similar to a less severe sore on the surface but hide severe damage beneath, possibly correlating to stage III or IV conditions.
Recognizing these signs can help in the prevention of pressure ulcers turning severe. Regular monitoring and early intervention by health care providers are essential for managing and treating these wounds.

Diagnosis and Assessment of Pressure Injuries
Pressure ulcers, also known as decubitus ulcers, need careful assessment by healthcare professionals. They examine the skin closely to diagnose pressure injuries and determine how severe they are. The severity is measured in "stages," which helps in deciding the right treatment plan. Pressure ulcers can be complicated, sometimes resulting in deep wounds and infections. Early diagnosis and proper staging are essential for effective care.
Staging System (Stage 1 to Stage 4)
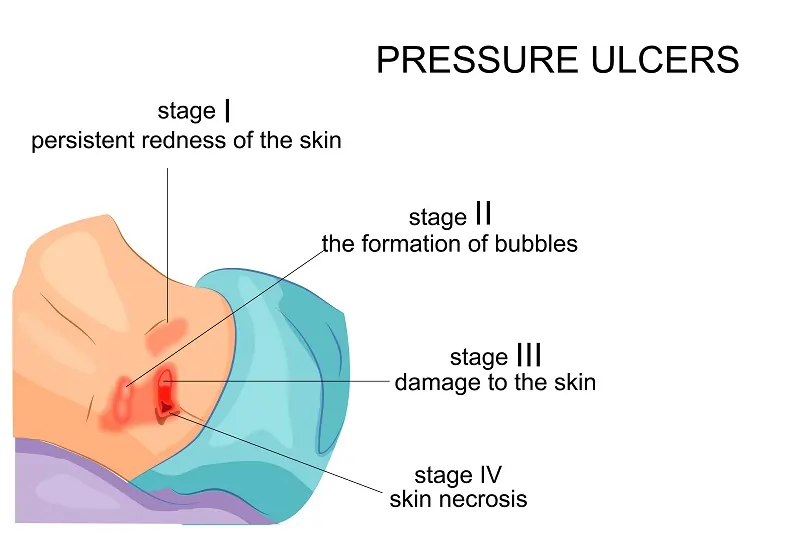
Pressure ulcers are graded in stages from 1 to 4:
- Stage 1: This is the mildest form. The skin looks red and doesn't turn white when pressed. You might feel pain, itchiness, or a change in skin temperature.
- Stage 2: Here, the skin breaks and a shallow open sore forms. Sometimes, fluid may leak from it. It's essential to clean the sore and use Foam dressings.
- Stage 3: The sore is deeper now, affecting all skin layers and some underlying tissue. It doesn't reach muscle or bone.
- Stage 4: This stage is the most serious. The ulcer is very deep, with extensive damage that reaches muscles and maybe bones. There is a risk of serious infections here.
The NPIAP System now considers injuries to both intact skin and open ulcers, highlighting the need for precise staging.
Tools for Diagnosis
To diagnose pressure ulcers, a healthcare provider will visually check the skin's condition. They use a structured staging system to guide treatment decisions. Blood tests are also helpful, showing the patient's overall health and nutritional status. They also assess risk factors like mobility, past history, and any incontinence issues. Monitoring involves looking for changes in skin color or texture. Patients are advised to use mirrors for hard-to-see areas.
In summary, diagnosing and staging pressure ulcers require thorough examination and careful grading. Quick detection and proper management can aid in the healing of pressure ulcers and prevent further complications.
Common Complications
Pressure ulcers can lead to serious health issues. One major complication is cellulitis, a skin infection that can spread to deeper layers and affect other body parts. If the ulcer reaches the bones or joints, it can cause infections that may damage cartilage and limit movement. Untreated pressure ulcers pose a risk of sepsis, a severe, body-wide infection that can lead to organ failure. Another serious condition is necrotizing fasciitis, a rapid skin infection causing tissue death. These complications not only disrupt recovery but can extend hospital stays and increase the risk of premature death.
Infection Risks
Bacterial infections are common with pressure sores and pose significant health risks. Signs of an infection include fever, chills, intense pain, bad odor, redness, warmth, swelling, and pus. Infections can spread from the surface to deeper layers, leading to cellulitis and potentially life-threatening conditions like sepsis. Sinus tracts, or deeper connections from the sores, can cause severe infections such as bacteremia and osteomyelitis. Prompt treatment is vital, as untreated sores can worsen, affecting bones, cartilage, and surrounding tissues.
Impact on Healing
Several factors can impact the healing of pressure ulcers. Prolonged bed rest increases the risk of respiratory issues and urinary tract infections (UTIs). Poor nutrition can make developing pressure sores easier and slow the healing of existing ones. Conditions like diabetes and vascular diseases impair healing and increase susceptibility to pressure injuries. Mechanical factors like pressure and friction, especially over bony areas, can cut off blood flow and complicate healing. Excessive moisture around sores can also delay healing and cause further skin breakdown.
Treatment Strategies
Caring for pressure ulcers, also known as decubitus ulcers, involves several key strategies. These include pressure relief, wound cleaning, dressing and bandaging, pain management, and nutritional support. Each approach is vital for healing and preventing further damage.
Pressure Relief Techniques
Relieving pressure is crucial for healing pressure injuries. Patients should be repositioned every 1 to 2 hours to avoid pressure build-up. Foam pads and specialty wheelchairs can help reduce stress on sore areas. Keep the head of the bed at less than 30 degrees to prevent pressure on the lower back and tailbone. Use pressure offloading surfaces, like specialized mattresses or cushions, to distribute weight evenly. Implement a schedule for position changes and use lifting devices to minimize friction and avoid skin injury.
Wound Cleaning Measures
Proper wound cleaning is essential for managing pressure ulcers. Irrigate the wound with saline or water during dressing changes to clear away debris. This helps prevent bacterial infections. Cleanse the wound carefully, especially if there is broken skin. Maintain a moist wound environment using dressings such as hydrogel, hydrocolloid, and foam. Debridement may be needed to remove dead tissue and promote healing. Regular dressing changes are important for monitoring signs of infection and ensuring healing.
Dressings and Bandaging of Pressure Ulcers
Choosing the right dressing is key for pressure ulcer management. Transparent films and hydrogels work well for protecting stage 1 sores. They should be changed every 3 to 7 days. Hydrocolloid patches are good for light drainage and can stay in place up to a week.
Alginates, made from seaweed, are designed for heavy drainage and need to be changed when saturated. Foam dressings suit various drainage levels and are changed every 3 to 4 days. Waterproof options are available to guard against moisture.

Pain Management Approaches
Managing pain is a significant concern in pressure sore care. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often preferred over opioids to avoid sedation. Patients can take NSAIDs before repositioning or wound cleaning. If infection occurs, antibiotics may be prescribed to manage pain. Topical pain relievers, prescribed by a doctor, can also be applied for discomfort. Severe cases may require debridement to remove dead tissue, aiding pain management and healing.
Nutritional Support
Nutrition plays a vital role in the healing of pressure ulcers. A high-protein diet is beneficial in preventing and healing sores. Many patients with pressure ulcers suffer from malnutrition, often due to age or health conditions. A nutrition specialist can provide an evaluation to enhance recovery. Supplementing deficient vitamins may be necessary for healing. In severe cases, enteral or IV nutrition might be required to ensure adequate nutritional intake.
Effective treatment of pressure ulcers requires a comprehensive and tailored approach, addressing all aspects of care to promote recovery and prevent further injury.
Prevention of Pressure Ulcers

Pressure ulcers, also known as bedsores or decubitus ulcers, affect over 2.5 million people yearly in the U.S. These ulcers occur when skin and underlying tissue are damaged due to prolonged pressure. They are frequent in people over 65, those with limited mobility, or those with nerve damage from spinal cord injuries.
To prevent pressure ulcers, regular repositioning, using cushions and mattresses designed to relieve pressure, and maintaining good nutrition are key. Common sites for pressure ulcers include the heels, sacrum, and hips, where bones are close to the skin.
Repositioning Techniques
Repositioning is crucial in preventing pressure sores. Those confined to bed should change positions every 1 to 2 hours. If seated in a chair, changing positions every hour is advised. Encourage individuals to shift their weight every 15 minutes if possible.
Caregivers should inspect the skin daily for redness or other early signs of pressure sores. This can prevent painful and severe pressure injuries. Techniques such as using pillows for support, weight shifting, and wheelchair pushups for those who can manage are effective.
Skin Care Routines
Skin care routines are vital for preventing pressure injuries. Start by inspecting the skin upon admission and continue daily, especially paying attention to areas under medical devices. Use pH-balanced skin cleansers and apply moisturizers after incontinence episodes to keep skin healthy.
Soiled areas should be washed immediately with warm water and soap to prevent infections, ensuring the skin is kept warm and dry. Moisture barrier creams can protect skin from irritants like urine and feces. Regular repositioning every two hours while in bed helps minimize pressure.
Lifestyle Modifications
Lifestyle changes can greatly lower the risk of pressure ulcers. Regularly changing positions is essential to relieve pressure on existing ulcers and prevent new ones. Specialized mattresses and cushions can significantly reduce pressure on vulnerable skin areas.
A balanced diet rich in nutrients supports skin health. Proper nutrition helps in maintaining a positive nitrogen balance, which is essential for skin repair. Staying active, as much as possible, supports circulation and reduces risks. Daily skin checks ensure any pressure-related issues are addressed early for effective management.
In summary, the prevention of pressure ulcers involves a combination of good repositioning, proper skin care routines, and lifestyle changes. By following these guidelines, we can greatly reduce the risk of developing these painful and costly wounds.
Importance of Multidisciplinary Care
Pressure injury prevention and treatment require the teamwork of many professionals. This collaborative approach ensures better care and safety for patients. An organization's culture and practices play a crucial role in promoting safety. Risk assessment helps identify patients at high risk for pressure injuries. This process requires input from various healthcare professionals. Nutritional assessment and repositioning are key interventions. An interdisciplinary approach is essential for effective pressure ulcer prevention.
Roles of Healthcare Professionals
Healthcare professionals are vital in assessing and treating pressure ulcers. They evaluate the skin's condition and assign the ulcer's stage. This evaluation helps in choosing the right treatment plan. An interdisciplinary approach improves hospital care for pressure ulcer prevention.
Regular skin checks by healthcare professionals allow for early detection and intervention. Treatments may include special mattresses, dressings, creams, or surgery in severe cases. Education on diet, activity, and position changes is emphasized for prevention.
Collaboration in Treatment
Treating pressure injuries requires team collaboration. Responsibility extends beyond nurses to the entire healthcare system. Risk assessment is crucial for early identification of at-risk individuals. Reducing pressure, managing pain, and preventing infection are key treatment strategies. A team may include primary care doctors, wound specialists, nurses, social workers, and physical therapists. Each member provides unique expertise. Collaborative efforts also address nutrition, repositioning, skin care, and emotional support for comprehensive patient recovery.
Recognizing When to Seek Medical Advice
Pressure ulcers, also known as pressure injuries or decubitus ulcers, need immediate attention. If you notice any symptoms, it's important to consult a health care provider right away. This can prevent complications and promote healing of pressure ulcers effectively.
Signs for Urgent Care
Recognizing signs that require urgent care can make a big difference in treatment outcomes. Here are key indicators to watch for:
- Hot, Swollen, or Red Skin: On brown or black skin, these areas may appear purple or blue.
- Presence of Pus: Pus or any unusual discharge is a serious sign. It may indicate bacterial infections.
- High Temperature: A sudden fever might suggest a systemic infection. This requires prompt attention.
- Severe or Worsening Pain: Significant pain can signal that the condition is getting worse.
- Unpleasant Odor: This may indicate deeper tissue damage or a critical infection.
In need of urgent care? Contact a health care provider or visit a GP practice without delay. Addressing these symptoms early is vital for effective management of pressure ulcers.