Chronic wounds pose a significant challenge in healthcare, affecting millions and often leading to severe complications. Understanding these non-healing wounds is crucial, as they can arise from various conditions, including diabetes, vascular diseases, and infections. This complexity necessitates a comprehensive approach to wound management and patient care.
The healing process is not merely a biological event but is influenced by a myriad of factors that can hinder recovery. From physiological stages of healing to external barriers such as environmental conditions and patient attributes every element plays a vital role in how wounds recover. Effective management strategies that consider these variables are essential for improving outcomes.
In this article, we will delve into the types and causes of chronic wounds, explore innovative treatment options, and highlight the importance of patient-centered care. By understanding the intricacies of chronic wound care, we can better equip ourselves to assist those affected on their journey to healing.
Understanding Chronic Wounds
Chronic wounds are injuries that don't heal within the usual time frame. Normally, these wounds take less than two weeks to heal. However, they can persist for weeks or even months in some cases, never fully recovering.
This condition can occur due to problems like disrupted blood flow or nerve damage. Treating these wounds is expensive, costing over $25 billion every year in the United States. Each diabetic ulcer, for example, can cost up to $50,000. Living with chronic wounds can be tough.
They often lead to physical pain, reduced mobility, and emotional stress, significantly impacting a person's quality of life. Managing these injuries is vital, particularly for older adults who are more affected by them. Each type of chronic wound needs specific care and prevention techniques.

Types of Chronic Wounds
Chronic wounds come in various types, each requiring distinct care. Here’s a quick overview of common types:
- Pressure Injuries: Occur on skin over bony prominences due to prolonged pressure.
- Diabetic Foot Ulcers: Caused by poor blood flow and nerve damage from diabetes.
- Venous Ulcers: Often found on legs due to blood flow problems, such as varicose veins.
- Arterial Ulcers: Result from a lack of blood supply due to conditions like high blood pressure.
- Compromised Surgical Wounds: Happen when surgical cuts don't heal properly.
Diabetic ulcers emerge in diabetes patients with poor circulation and immune function. Venous ulcers, the most common type, are due to issues like deep vein thrombosis. Chronic wounds are those that fail to shrink by at least 15% each week or 50% in a month, making them stubborn and hard to treat.
Causes of Non-Healing Wounds

Non-healing wounds are a problem when there's no improvement after two weeks or no full healing in six weeks. Many factors delay healing. Poor blood flow, nerve damage, and various health conditions can all contribute. These factors disrupt normal wound healing phases. For example, during the inflammatory phase, the body releases substances that cause redness and swelling, which is necessary for healing. But, excessive inflammation can impede progress.
Crucial agents in this process include:
- Neutrophils: Fight bacteria.
- Monocytes/Macrophages: Produce growth factors for tissue regeneration.
Chronic wounds continue to present challenges due to their complexity. They drain patient resources and healthcare systems because of the prolonged treatment required. Understanding these contributing factors is essential to improve care and solutions.
Physiological Healing Processes
Chronic wounds, like pressure ulcers, diabetic foot ulcers, and venous leg ulcers, need special care to heal properly.
To restart the healing process, several factors are crucial. These include continuous blood flow, infection prevention, a moist environment, and cleaning out dead tissue. These conditions help new skin and tissues grow effectively. When chronic wounds show no improvement in two weeks or do not heal in six weeks, they are called non-healing wounds. These can lead to serious issues such as illness or even limb loss. It is essential to give these wounds timely and effective care to avoid further complications.
Stages of Wound Healing
The healing of wounds happens in three stages: inflammatory, proliferative, and remodeling. The inflammatory phase starts soon after the wound closes. In this stage, the body works to clean the wound by sending white blood cells to fight infection. Cytokines, small proteins, help by attracting other cells needed for repair. The hemostatic part of this phase prevents blood loss by forming clots. Healing requires a steady supply of nutrients and other essential elements. They ensure the healing continues smoothly through all phases.
Factors Affecting Healing
Several factors can influence whether a chronic wound heals well. Proper blood flow, good nutrition, and infection control are key. A moist environment and removing dead tissue also help. Nutrients like proteins, vitamins A and C, and zinc play an important role. Wounds heal better when there is proper blood circulation and a strong immune system. Chronic wounds may result from poor circulation, prolonged immobility, or conditions like diabetes. If a wound does not improve in two weeks or fails to heal in six weeks, it is a chronic wound. Such wounds often need special treatments to trigger healing.
Barriers to Effective Wound Healing
Chronic wounds can be stubborn and tough to heal. These wounds often stem from issues like tissue necrosis, where cells die due to a lack of blood flow or injury. When this happens, it can lead to long-lasting ulcers that are difficult to treat. A person's nutrition also plays a big role. Lacking proteins and key vitamins, such as A, C, and zinc, can slow down how fast a wound heals. Oxygen is vital for healthy healing. When there isn't enough, due to poor blood flow, especially in extremities like feet or hands, wounds can get worse. Also, wounds can become more serious when infection sets in. In such cases, using cleansing agents and topical antimicrobials can help clear infections and encourage healing.
Patient Factors
Patients with chronic wounds face several personal challenges. Many deal with limited movement and constant pain, affecting their jobs and social lives. One diabetic ulcer can cost up to $50,000, showing how expensive treatment can be. This financial strain can lead to feelings of isolation for many, impacting their mental health. The cost of managing venous leg ulcers in the U.S. is huge—$14.9 billion a year. This hits the healthcare system hard and also burdens patients. Because chronic wounds need long-term care, the costs can mount quickly. With emergency and inpatient care, this might reach $3 billion over ten years.
Environmental Factors
Environment impacts how wounds heal. If pressure stays on the same spot too long, it can lead to pressure ulcers. This happens when the pressure is stronger than the blood capillaries can handle. Other factors like constant moisture, shearing, and heat make matters worse. Humidity plays a big role, too. At a high humidity level, the skin's protective layer becomes much weaker. At 100% humidity, it's 25 times more fragile than at 25%. Likewise, skin becomes four times more fragile at 95°F than at 86°F. Keeping wounds in a moist environment, however, can be helpful. Moisture supports tissue growth and repair, aiding the healing process.
In summary, understanding these factors is key to improving the healing of chronic wounds. Proper care can make a huge difference in outcomes and patients' quality of life.
Management Strategies
Chronic wounds need constant attention and a mix of management methods. These include topical care and sometimes surgery, depending on the wound. Proper management of chronic wounds, like pressure ulcers, diabetic foot ulcers, and venous leg ulcers, requires specific plans tailored to each wound type.
Key to healing is ensuring good blood flow, nutrition, infection control, and a moist environment. Removing dead tissue is also crucial for new tissue growth.
Older adults are more affected by chronic wounds, making it vital for all healthcare providers to know how to prevent, identify, and treat these wounds. Managing patients with chronic wounds is challenging due to recurring issues and increased morbidity, demanding a comprehensive approach.

Wound Assessment Techniques
Chronic wounds often do not heal due to lack of blood, oxygen, or nutrients, and an environment that promotes infection. Factors like comorbidities, body mass index, wound location, and medication affect healing time. A wound is called chronic if it does not reduce in size by 15% weekly or 50% monthly. Wound care involves debridement and selecting the right dressings based on tissue perfusion, immune strength, hydration, and infection control.
Wound Care and Dressing Choices
Chronic wounds are often treated with moist dressings chosen based on wound type and severity. In 2015, pressure injuries occurred in about 8.8% of US care facilities, pointing to the need for effective dressings. New dressings, like self-healing hydrogels and hydrocolloids, are improving healing.
The TIME framework helps choose the right dressing by focusing on Tissue, Infection, Moisture imbalance, and Edge advancement. Technology-enabled dressings with biosensors and drug delivery systems can enhance treatment by allowing real-time monitoring.
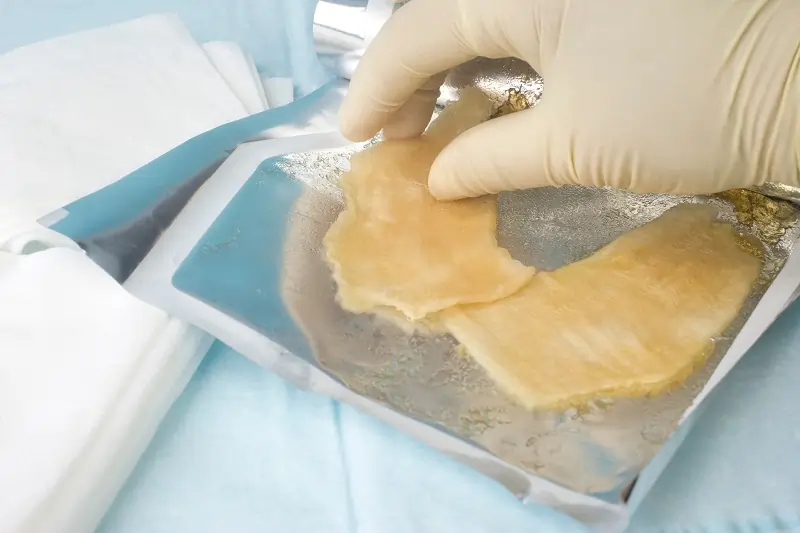
nnovative Treatments
Recent innovations in wound care have shifted to advanced options such as self-healing hydrogels and bioengineered skin substitutes, which can boost healing. Advanced dressings now include biomarkers and biosensors, creating a theranostic approach for better chronic wound treatment. Techniques like 3D printing and e-skin therapy offer tailor-made solutions for patients. Modern dressings with power sources and interfaces like Bluetooth support on-demand drug delivery and patient monitoring. These cutting-edge dressings improve compliance, cost-effectiveness, and durability, highlighting the significance of smart formulations in managing chronic wounds.
Dressing Types and Functions
| Dressing Type | Function |
|---|---|
| Hydrogels | Maintain a moist environment for tissue growth. |
| Hydrocolloids | Protect wounds and absorb exudate. |
| Foam Dressings | Provide cushioning and absorb moisture. |
Patient-Centered Care
Patient-centered care is vital for managing chronic wounds. Treatment plans should be personalized based on each patient's history and current conditions. This ensures that care aligns with personal preferences and improves outcomes. Follow-up care must be tailored to each patient's health needs. It is important for patients to understand the next steps and to have details about follow-up appointments before leaving the clinic.
The management of chronic wounds often involves a team of healthcare professionals. These teams collaborate to provide the best personalized care and support options. Listening to the experiences of those living with chronic wounds helps healthcare providers focus on person-centered approaches. This enhances patient wellbeing and recovery. Ongoing assessments are also crucial. They help address the unique challenges each patient faces during their treatment journey.
Importance of Self-Management
Educating patients on self-management is crucial for chronic wound care. It empowers them to take control of their healing process. Proper nutrition plays a significant role in self-care for slow-healing wounds. The body needs adequate nutrients to heal efficiently. Patients should avoid medications like anti-inflammatories that can hinder natural healing.
It's also important to understand the health history and lifestyle factors related to chronic wounds. This helps in developing personalized self-care strategies that overcome healing barriers. Engaging in person-centered care improves overall wellbeing and fosters better self-management practices.
Educating Patients on Wound Care
Chronic wounds are common, especially among older adults. It's vital for healthcare providers from all specialties to know how to prevent, identify, classify, and treat these wounds. Personalized treatment is key and should consider the patient's unique health history and preferences.
Evidence-based management improves outcomes, underscoring the need for specialized training among clinicians. Effective communication between patients and healthcare providers enhances wellbeing and healing. Follow-up care should be personalized, coordinating necessary supplies and clearly communicating future steps and appointments.
Advanced Dressing Technologies
Advanced dressing technologies are improving chronic wound care significantly. These dressings include nanofibers, hydrogels, and collagen-based products. Here's a closer look at their benefits:
- Polymeric Nanofibers: Loaded with antibacterial agents, these dressings help fight antibiotic resistance. They are particularly useful in treating infected wounds.
- Green Tea-infused Hydrogels: These smart dressings are designed for chronic diabetic wounds. They offer unique properties that aid in faster healing.
- Biomechanically Active Hydrogels: These dressings not only speed up wound closure but also support healing through a coordinated biochemical approach.
- Collagen Products: Ideal for chronic and non-healing wounds, collagen attract essential cells and reduce harmful elements like free radicals.
- Variety of Dressings: Options like films, hydrocolloids, and foams are available to suit different wound conditions, increasing the efficacy of treatment.
| Dressing Type | Benefits |
|---|---|
| Polymeric Nanofibers | Combats antibiotic resistance |
| Green Tea-infused Hydrogels | Enhances healing for diabetic foot ulcers |
| Biomechanically Active Hydrogels | Accelerates wound closure |
| Collagen Products | Attracts cells and neutralizes free radicals |
These advanced dressings are instrumental in treating chronic wounds, improving patient outcomes, and enhancing the quality of life.
When to Refer to a Specialist
Chronic wounds require timely and specialized care to prevent complications. A wound is considered chronic if it shows no signs of healing after 4 to 12 weeks of treatment. In such cases, it's essential to refer the patient to advanced wound care.

Key signs to contact a wound care specialist:
- Increased pain: A sudden rise in pain levels can signal an underlying issue.
- Discharge or pus: Any unusual discharge may indicate an infection.
- Fever: This can be a sign of a systemic infection needing immediate attention.

A multidisciplinary team is vital for chronic wound management. This often includes wound care specialists, podiatrists, and vascular surgeons. Their combined expertise can address various challenges related to healing.
Regular follow-ups are crucial for monitoring progress and adjusting treatment strategies. Additionally, psychological support may help those dealing with the stress of non-healing wounds.
Here’s a quick overview:
| Symptom | Action |
|---|---|
| No healing for 4-12 weeks | Refer to a specialist |
| Increased pain | Seek medical attention |
| Discharge or pus | Contact a doctor |
| Fever | Immediate medical care |
Proactive referral to a specialist can save time and potential complications, boosting the patient's quality of life.
Conclusion and Future Directions in Chronic Wound Care
Chronic wound care is a complex field requiring personalized treatment plans. Considering the patient's diagnosis, health history, and preferences can lead to effective care. Collaboration among healthcare professionals is essential for addressing the diverse needs of patients.
Hyperbaric oxygen therapy has emerged as a beneficial option. It enhances wound healing by delivering oxygen to affected areas through specialized oxygen chambers. This method may play a significant role in future treatment strategies.
The burden on healthcare systems is substantial, with costs exceeding $25 billion annually. This figure is expected to rise as diabetes prevalence increases. Therefore, innovative and cost-effective solutions are crucial.
Research and evidence-based practices are vital. They ensure clinicians use the most current and effective methods. Staying updated with new findings will improve patient outcomes and quality of life.
Future Directions in Chronic Wound Care:
- Integrating technology: Use of digital tools for monitoring and treatment.
- Improving interdisciplinary collaboration: More teamwork among specialists.
- Expanding research and trials: Ongoing studies for innovative therapies.
These efforts can lead to better chronic wound management and patient care.