Introduction to Wound Healing Process
The wound healing process is divided into three overlapping phases: the inflammatory stage, fibroblastic stage, and maturation stage.
During the inflammatory stage, blood vessels constrict to minimize blood loss, and immune cells are activated to respond to injury. This phase is crucial for preventing infection and initiating healing.
Next is the fibroblastic stage, characterized by collagen growth and the formation of new tissue. Fibroblasts proliferate, producing collagen that helps to bridge the wound, providing strength and structure to the healing tissue.
Finally, the maturation stage involves the refinement of collagen, where it becomes more organized, and scars begin to fade. Over time, the remodeled tissue gains strength and functionality, although it may not fully match the original skin.
Disruptions in any of these stages can lead to abnormal healing outcomes, such as excessive scar formation or chronic wounds.
Proper healing relies on the seamless transition from one stage to another, highlighting the importance of each phase in the overall recovery process.
Specific Wound Healing Phases
Wound healing is a complex physiological process that occurs in a series of well-defined phases, each critical for restoring tissue integrity and function. Understanding these specific phases hemostasis, inflammation, proliferation, and remodeling provides valuable insights into how the body responds to injury and how various factors can influence recovery outcomes.
During hemostasis, the body works to stop bleeding and form a clot, while inflammation sets the stage for healing by cleaning the wound of debris and pathogens. The proliferation phase involves the formation of new tissue, utilizing collagen and extracellular matrix to rebuild structures. Finally, the remodeling phase strengthens and matures the new tissue, ensuring it can withstand normal stresses. Together, these phases highlight the intricate and dynamic nature of wound healing, emphasizing the importance of timely and appropriate care to promote optimal recovery.
Step 1: Stopping the bleeding (hemostasis)

Hemostasis is the critical initial stage of wound healing, aimed at stopping bleeding. When a blood vessel is injured, it undergoes vasoconstriction, reducing blood flow to the area. This response is quick, minimizing blood loss. Concurrently, platelets adhere to the exposed collagen fibers at the wound site, becoming activated and aggregating to form a plug – a crucial step in clotting.
As platelets gather, they release chemical signals that recruit even more platelets, enhancing clot formation. This aggregation is further stabilized by fibrin, a protein that weaves through the platelet plug, forming a mesh-like structure that solidifies the clot. The fibrin not only strengthens the clot but also serves as the foundation for a scab, which protects the wound from external contaminants and further injury.
The hemostatic process is vital, as it prevents excessive blood loss and sets the stage for subsequent phases of healing. By stopping the bleeding and providing a scaffold for tissue repair, hemostasis plays a fundamental role in the body’s natural
Step 2: Inflammation
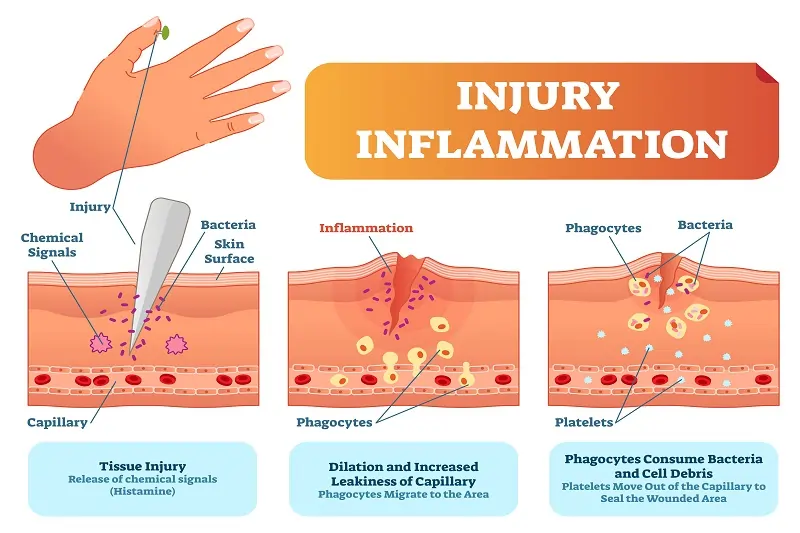
The Inflammatory Phase of wound healing is crucial for initiating the repair process. During this phase, macrophages and white blood cells (WBCs) play a vital role in fighting infection and promoting tissue repair. Upon injury, blood vessels constrict briefly, but soon dilate, allowing WBCs to migrate to the wound site. Macrophages are particularly important as they engulf pathogens and cellular debris, releasing cytokines that attract more immune cells to the area.
The release of chemicals by blood platelets, such as histamine and prostaglandins, triggers inflammation. This response results in the classic signs of inflammation: redness, swelling, heat, and pain. Redness and heat are due to increased blood flow, while swelling arises from the accumulation of fluid and immune cells. Pain is mediated by chemicals that stimulate nerve endings.
As macrophages continue to secrete growth factors, they not only facilitate the healing process by stimulating cell proliferation and tissue repair but also help transition the wound to the next healing phase. This inflammatory response is essential for creating an environment conducive to healing and preventing infections.
Step 3: Growth and rebuilding
During the third phase of wound healing, known as growth and rebuilding, oxygen-rich red blood cells (RBCs) play a pivotal role in tissue regeneration. As the body responds to injury, RBCs are delivered to the site through an enhanced blood supply, delivering essential oxygen and nutrients that are critical for cellular functions.
Chemical signals, such as growth factors and cytokines, are released at the wound site to mobilize fibroblasts and other key cells. These signals instruct fibroblasts to produce collagen, a vital protein that acts as a scaffold for new tissue formation. Collagen provides structural support, facilitating the binding of cells and aiding in the reconstruction of the damaged area.
As healing progresses and new tissue develops, collagen deposition leads to the appearance of a scar. Initially, scars are often red and raised due to the influx of blood vessels; however, over time they mature, becoming flatter and paler as collagen is remodeled and the vascularity decreases. This intricate process of growth and rebuilding underscores the body's remarkable capacity to heal itself after injury.
Step 4: Strengthening
After a wound has initially healed, the process of strengthening the scar tissue begins. In the first six weeks, the new tissue gains strength rapidly as collagen fibers reorganize and cross-link, providing structural support. By three months post-injury, the scar reaches approximately 80% of its original strength.

may indicate the strengthening process: patients often experience stretching and itching as the tissue adjusts. Puckering can also occur as the skin settles into place, marking the dynamic nature of healing. It’s important to note that while the scar tissue becomes stronger, it never fully regains the original strength of uninjured skin.
This ongoing maturation involves the gradual remodeling of collagen, which continues for up to a year or more. Proper care during this phase can enhance the quality of the scar and minimize discomfort, allowing the healing process to advance efficiently. Understanding this strengthening process is essential for optimal recovery and long-lasting results.
Wound Healing Dressings

Wound healing dressings play a pivotal role in the recovery process, emphasizing essential characteristics like wound protection, maintenance of a humid environment, and high permeability to oxygen. These dressings create a barrier against external contaminants while allowing the skin to breathe, which is crucial for effective tissue repair.
Modern wound dressings are engineered to facilitate healing by promoting organized cellular and molecular mechanisms. They maintain a moist wound environment, which is essential for cell migration and proliferation, thereby accelerating the healing process. Ensuring high oxygen permeability further enhances tissue oxygenation, supporting metabolic activities essential for recovery.
Additionally, many dressings are embedded with antimicrobial agents to prevent infection, thus reducing the risk of complications that can impede the healing process. By combining these features wound protection, a humid environment, optimal oxygen levels, and infection prevention—modern wound dressings significantly improve patient outcomes and foster effective tissue repair.
Wound Healing Providers
Wound healing involves a multidisciplinary team of providers, each specializing in different aspects of the healing process. Physicians, particularly those in wound care, dermatology, and plastic surgery, assess and treat various wound types, from surgical incisions to diabetic ulcers. Nurse practitioners and wound care nurses play a vital role in day-to-day management, dressing changes, and patient education, ensuring optimal care and compliance.
Physical therapists contribute by improving mobility and circulation, while dietitians focus on nutritional support to enhance healing. Additionally, pharmacists may recommend topical treatments and manage pain associated with wounds.
These providers oversee the stages of healing— inflammation, proliferation, and remodeling—ensuring the body responds effectively and preventing complications like chronic wounds. Their collective expertise is crucial in identifying infection, addressing underlying conditions, and implementing proactive interventions to foster healing. Through collaborative management, wound healing providers not only promote recovery but also enhance quality of life for patients, ultimately reducing the risk of chronic wounds.
Wound Healing Prognosis
Wound healing prognosis is influenced by several factors, largely determined by the three primary wound healing phases: the inflammatory phase, fibroblastic phase, and remodeling phase.
The inflammatory phase initiates the healing process, characterized by increased blood flow and immune response to prevent infection. Any delay or complication here can lead to prolonged healing. The fibroblastic phase involves collagen deposition and tissue regeneration, crucial for tissue strength and integrity. A disrupted fibroblastic phase can significantly extend recovery time and negatively affect the outcome. Finally, the remodeling phase refines and strengthens the scar tissue, often lasting months to years; successful completion is vital for the functional restoration of the tissue.
Signs of wound healing problems include persistent redness, increased pain, excessive swelling, or the presence of necrotic tissue, which all indicate deviations from normal healing processes. Recognizing these issues early is essential for improving prognosis and guiding appropriate interventions to facilitate recovery.
Wound Healing Process Summary
In conclusion, the wound healing process progresses through several key stages: hemostasis, inflammation, tissue growth, and scar formation.
Overall, the wound healing process is vital for recovery, with inflammation and granulation playing crucial roles in restoring skin integrity and firmness over time.